 Many people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and long COVID feel extreme exhaustion that does not improve with rest. Even small amounts of physical or mental activity can make symptoms much worse for days or weeks. Scientists are now finding strong evidence that this may be linked to problems in the body’s energy-making system—the mitochondria.
Many people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and long COVID feel extreme exhaustion that does not improve with rest. Even small amounts of physical or mental activity can make symptoms much worse for days or weeks. Scientists are now finding strong evidence that this may be linked to problems in the body’s energy-making system—the mitochondria.
This blog explains what mitochondria do, what may go wrong in ME/CFS and long COVID, and why this matters for patients and clinicians.
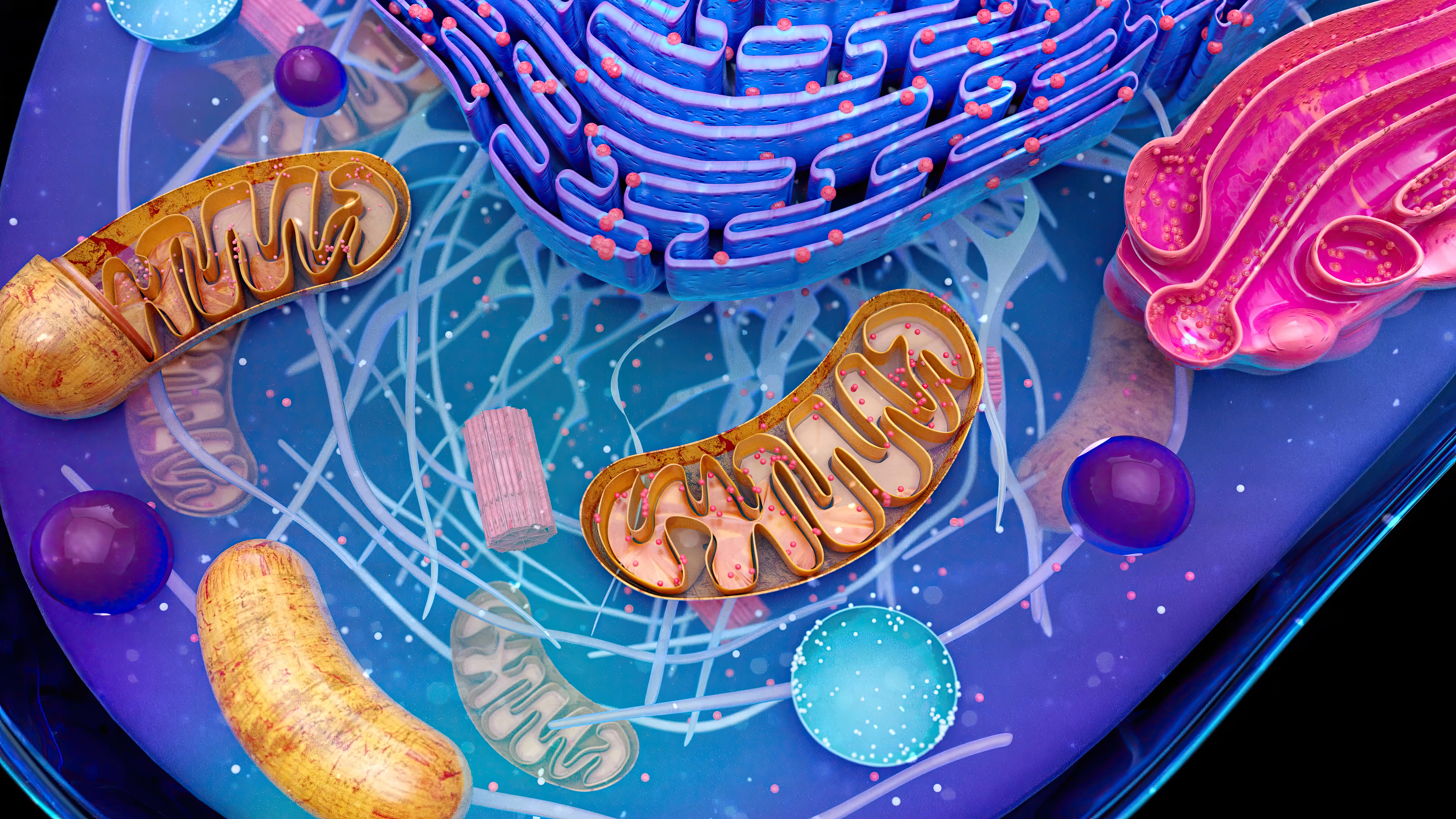
What Are Mitochondria?
Mitochondria are tiny structures inside our cells. They are often called the “power plants” of the cell because they make ATP, the molecule that provides energy for:
- Muscle movement
- Brain function and thinking
- Immune system activity
- Recovery after exercise
Healthy mitochondria help the body switch smoothly between rest and activity.
What Is ME/CFS?
ME/CFS is a long-term illness that affects many systems in the body. Common symptoms include:
- Severe fatigue lasting more than 6 months
- Post-exertional malaise (PEM) — symptoms worsen after activity
- Brain fog (trouble thinking or concentrating)
- Poor sleep
- Dizziness or heart rate changes
- Pain
ME/CFS affects women more often than men and has no single diagnostic test.
Why Mitochondria Matter in ME/CFS
Many studies show that people with ME/CFS have signs of mitochondrial dysfunction, meaning their cells struggle to make energy efficiently.
Researchers have found:
- Slower energy recovery after exercise
- Lower ATP production in muscles and blood cells
- Higher lactic acid levels (a sign of poor oxygen use)
- Increased oxidative stress, which damages cells
This helps explain why people with ME/CFS may feel exhausted after even mild activity.
Oxidative Stress: When Cells Are Overloaded
When mitochondria do not work properly, they can produce too many reactive oxygen species (ROS). These are harmful molecules that damage proteins, fats, and DNA.
In ME/CFS, studies show:
- Higher levels of oxidative damage
- Lower levels of antioxidants like Coenzyme Q10 (CoQ10)
- Ongoing stress on cells and tissues
This creates a cycle where damaged mitochondria cause more stress, and more stress causes further damage.
A New Clue: ER Stress and a Protein Called WASF3
Recent research has identified a new possible player in ME/CFS called WASF3.
What is ER Stress?
The endoplasmic reticulum (ER) is another cell structure that helps make proteins. When cells are under stress—such as during infections—the ER can become overwhelmed. This is called ER stress.
Viruses are known to cause ER stress, which may help explain why ME/CFS and long COVID often begin after infections.
What Does WASF3 Do?
WASF3 is a protein that normally helps control cell shape and movement. However, researchers found that when WASF3 levels become too high:
- Mitochondria stop working efficiently
- Energy production drops
- Cells shift toward inefficient “emergency” energy use
- Exercise capacity decreases
In muscle samples from people with ME/CFS, WASF3 levels were higher than normal.
Why This Matters for the Immune System and Brain
Mitochondria are essential not just for muscles, but also for:
The Immune System
- Immune cells need energy to fight infections
- Poor mitochondrial function may cause chronic inflammation
- This could explain flu-like symptoms and PEM
The Brain
- Brain cells use large amounts of energy
- Mitochondrial problems may contribute to brain fog, memory issues, and headaches
What About Long COVID?
Long COVID shares many symptoms with ME/CFS, including:
- Severe fatigue
- PEM
- Brain fog
- Muscle weakness
New studies show that people with long COVID also have:
- Mitochondrial problems in muscle
- Increased reliance on inefficient energy pathways
- Poor recovery after activity
This suggests ME/CFS and long COVID may share similar underlying biology.
Can Mitochondria Be Treated?
There is currently no cure for ME/CFS, but many studies have tested treatments that support mitochondrial function.
Some supplements studied include:
- CoQ10
- NADH
- L-carnitine
- D-ribose
- Methylene blue
- Alpha lipoic acid complex
Some studies report symptom improvement, but results vary with use of these supplements alone.
Importantly, these approaches do not treat the root cause, which is still being studied.
Why This Research Is Important
Understanding mitochondrial dysfunction—and proteins like WASF3—may help researchers:
- Identify better biomarkers for diagnosis
- Develop more targeted treatments
- Explain why symptoms worsen after exertion
- Connect ME/CFS and long COVID under shared mechanisms
This research moves ME/CFS away from being misunderstood as “just fatigue” and toward being recognized as a biological, multi-system illness.
Citation: Syed AM, Karius AK, Ma J, Wang PY, Hwang PM. Mitochondrial Dysfunction in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Physiology (Bethesda). 2025 Jul 1;40(4):0. doi: 10.1152/physiol.00056.2024. Epub 2025 Feb 17. PMID: 39960432; PMCID: PMC12151296.
Image credit: julos freepik.com
