By Kathryn Boulter, ND | August 29, 2025
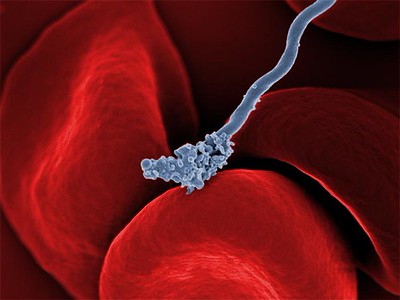
Lyme disease is a tick-borne illness caused by the bacterium Borrelia burgdorferi, with cases steadily rising in many parts of the world, particularly in the U.S. As tick populations expand and their geographical range increases, awareness about Lyme disease—and how to properly diagnose it—is more important than ever.
But Lyme disease testing is rarely straightforward. Multiple factors influence accuracy, and both mainstream and specialty guidelines offer different approaches. In this post, we’ll explore current testing methods, compare CDC and ILADS guidelines, review the role of co-infections, and highlight specialty diagnostic options such as IGeneX and Galaxy Diagnostics.
Why Lyme Disease Testing Matters
If you’ve been bitten by a tick or live in an area where Lyme disease is common, testing may help confirm or rule out infection. Early Lyme disease often resembles other illnesses, with flu-like symptoms such as fatigue, fever, headache, and muscle aches. The hallmark “bullseye” rash occurs in fewer than 50% of cases, making it unreliable as a stand-alone diagnostic tool.
When left untreated, Lyme disease can progress and cause significant complications—including joint pain, neurological issues, chronic fatigue, and heart problems. To complicate matters further, there are differing opinions on what tests should be run and how to interpret the results. Three major organizations—the CDC, IDSA, and ILADS—have each developed their own testing guidelines.
The CDC’s Two-Stage Testing Process
The CDC recommends a two-tiered approach to Lyme testing:
- Enzyme-Linked Immunosorbent Assay (ELISA) – This initial test detects antibodies (IgM and IgG) against Borrelia burgdorferi. However, false positives can occur, particularly in areas where other bacteria or viruses are common.
- Western Blot Test – If the ELISA result is positive or equivocal, a Western Blot is performed for confirmation. This test identifies specific proteins associated with Borrelia burgdorferi.
Both tests have significant limitations—especially during the early stages of infection, when the body may not yet have produced detectable antibodies.
Limitations of CDC Testing
The CDC’s protocol has been widely criticized for missing diagnoses, particularly in early-stage or atypical cases. Some patients never develop detectable antibodies in the first weeks of infection, while others with late-stage or post-treatment Lyme disease may test negative or equivocal despite ongoing illness.
These tests also do not screen for tick-borne co-infections, which are often transmitted alongside Borrelia burgdorferi and may require different treatment strategies.
ILADS Guidelines: A Broader Perspective
The International Lyme and Associated Diseases Society (ILADS) recommends a more comprehensive and clinically driven approach. Rather than relying solely on laboratory results, ILADS encourages providers to consider symptoms, patient history, and exposure risk.
ILADS recommends:
Testing for co-infections – Recognizing that ticks often carry additional pathogens such as Babesia, Anaplasma, Ehrlichia, and Bartonella, all of which may complicate diagnosis and treatment.
Clinical diagnosis – Evaluating symptoms such as fatigue, joint pain, and neurological issues in the context of tick exposure.
Extended testing – Using more sensitive tests, especially for patients with long-standing or atypical symptoms.
Tick-Borne Co-Infections: The Hidden Factor
Lyme disease is often only part of the picture. Ticks can transmit multiple pathogens, and co-infections may overlap with or mimic Lyme symptoms.
For example, Babesia can cause fever, chills, and fatigue similar to Lyme disease but requires an entirely different treatment protocol. Because standard CDC testing does not screen for these infections, persistent or unexplained symptoms after Lyme treatment may warrant co-infection testing.
Specialty Testing: IGeneX, Galaxy Diagnostics, and More
Growing recognition of the complexity of tick-borne illness has led to the development of specialized laboratories. IGeneX and Galaxy Diagnostics are among the best known, offering highly sensitive tests for both Lyme and co-infections.
Other notable labs include Medical Diagnostic Laboratories (MDL), TLab, and InfectoLab. These labs employ advanced technologies and testing strategies designed to detect infections that conventional tests may miss, making them particularly valuable for patients with chronic, atypical, or unresolved symptoms.
Conclusion: A Comprehensive Approach to Diagnosis
Lyme disease testing is rarely straightforward. While the CDC’s two-tier system remains the standard, its limitations—especially for early infections and co-infections—are clear. ILADS’ broader, symptom-driven framework emphasizes the importance of clinical judgment combined with expanded testing options.
For patients struggling with chronic symptoms or unclear diagnoses, specialty labs like IGeneX and Galaxy Diagnostics can provide more advanced insights. By integrating clinical evaluation with both traditional and specialized testing, providers can more accurately identify Lyme disease and co-infections, ensuring that patients receive the most effective treatment possible.
If you suspect Lyme disease or another tick-borne illness, it’s critical to work with a healthcare provider experienced in both conventional and specialty testing to develop an accurate diagnosis and effective treatment plan.
<-Back
- Image credit: “Borrelia-theileri-cow” by Alan R Walker is licensed under CC BY-SA 3.0. ↩︎
- Image Credit: “Borrelia hermsii Bacteria” by National Institutes of Health (NIH) is marked with Public Domain Mark 1.0. ↩︎